What is Cerebral Palsy?
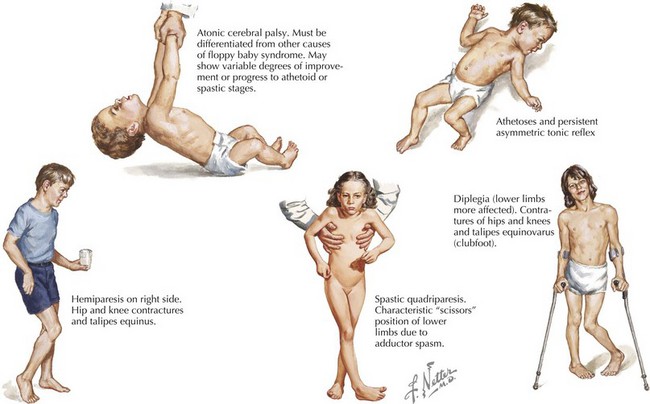
Cerebral palsy, commonly known as a physical disability that affects movement and posture, is a non-progressive motor control disorder that is most distinguishable by observing a general lack of muscle control and tone. Not only does it affect the person’s ability to move but also the individual’s coordination, reflexes, balance, swallowing, breathing, eating as well as neck, head and bowel control. Everyday tasks are difficult for people with cerebral palsy and constant therapy and care is needed.
It is the overarching term for a range of motor disorders that usually begin in the early stages of life, either before, during or after birth, and is usually a result of a brain injury. Although the cause is non-explicit and unclear, development abnormalities, asphyxia, infection, trauma or implications during labour are often associated with cerebral palsy.
Some symptoms include:
- Muscle tone variations that might see individuals being ‘floppy’ or overly stiff
- Muscle spasms or feeling stiff
- Favouring one side over the other
- Excessive drooling or swallowing abnormalities
- Delayed development where the baby or child is slow to reach common milestones like walking by 12-18 months and not speaking sentences by 24 months
- Seizures
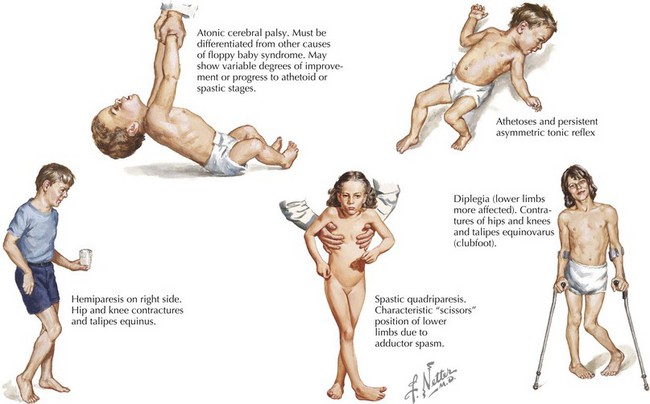
Photo credit: Obgyn Key
Management of Cerebral Palsy
The main goal of treating people with cerebral palsy is improving their quality of life by reducing the extent of their disability. Since there is currently no cure or direct treatment of the brain, modalities such as myofascial release, physiotherapy, orthotics and other assistive devices such as chairs and walking aids are used.
The benefits of myotherapy or myofascial trigger point therapy is that they can be used to improve function and delay the potential need for surgical intervention to treat fixed deformities – it is common for children with cerebral palsy to experience asymmetric pulling of muscle groups which could lead to scoliosis, subluxation or dislocation of their hips and inevitably, pain.
A study by Whisler et al., 2012, that considered the effects of myofascial release and other myofascial therapies on children with cerebral palsy, showed a dramatic improvement in body tone, range of motion, teeth grinding, ambulation, alertness, self-stimulatory activity and overall cooperation with therapists. In addition to this, the caregivers of the cerebral palsy children reported improvements in bowel movements without laxatives, their ability to lie supine with both hips flat on the bed, tolerance to touch, their need to be in self-protecting fetal position, ability to reach for objects and their ability to communicate with body language.
The myo therapy intervention used involved a myotherapist using trigger point therapy along points on the spine, neck and head, pressure and active isolated stretching on the extremities as well as non-invasive facial release in a clockwise direction from the ascending colon to the descending colon for 6 weeks. The intervention was then taught to the children’s caregivers to continue for weeks after.
Myotherapy for cerebral palsy using myofascial trigger pointing is postulated to improve fascial strain, abnormal muscle tone, a more normal 3D alignment and overall improved muscle function.